RamaOnHealthcare August 10, 2022
The Next Frontier of Health Data
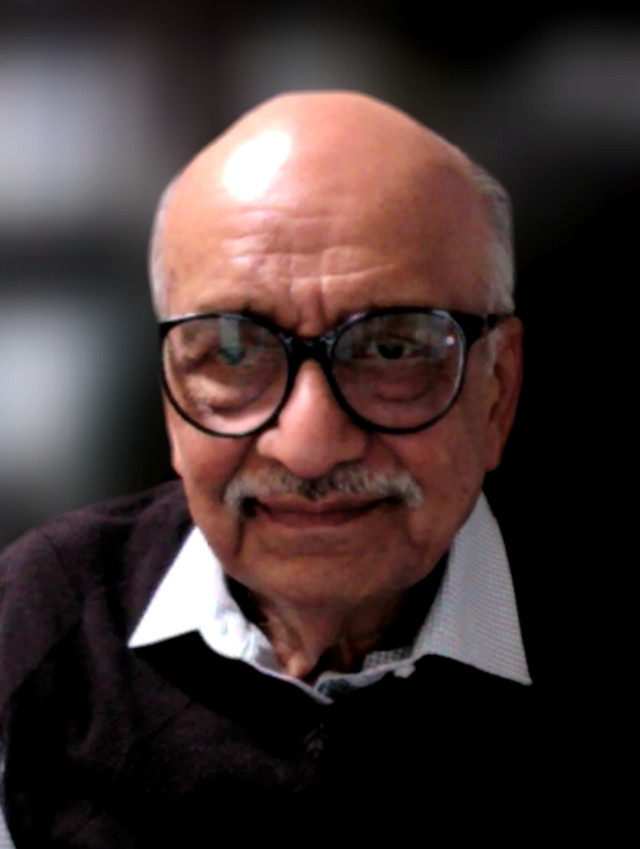
Today, RamaOnHealthcare talks with Ramesh Jain, the Founding Director of the Institute for Future Health at UCI. His imminent Personal Health Navigator (PHN) provides personalized health guidance while changing the focus from illness to maintaining/monitoring ongoing health and the potential to integrate user-generated data into medical records.
RamaOnHealthcare (ROH): Please explain multimodal data and its function or application within healthcare as a patient, industry, and physician.
Ramesh Jain (RJ): Health of an individual should be a unique, enjoyable journey, not a sequence of unpleasant disease episodes. Since lifestyle and environment are the most critical factors in a personal health journey, quantitative approaches for guiding food and lifestyle decisions while managing the environment are essential for achieving the desired quality of life and health. Our Personal Health Navigator (PHN) is imminent and will provide the proper guidance at the right time and form to any individual.
Today, wearable devices provide information related to lifestyle, activity, environment, and various biomarkers. Information regarding this personalized data is routinely gathered and available through mobile phones and websites for tracking and visualization. This promotes patient comprehension of their ongoing health state, offers personalized health data from disparate sensors, and provides the entry of multimodal health data via technology.
As Healthcare Providers within typical healthcare settings, an individual’s health is determined via various lab and radiological tests, blood pressure and pulse measurements, and the patient’s visual, physical, and verbal assessments. Professionals within Public Health may also emphasize social determinants of health (SDOH) to appreciate better the external state and environmental factors that impact individual and community health. Including personalized daily data from a patient’s cell phone adds another dimension and broader view of standard metrics. This changes the focus from treating ailments to supporting ongoing health.
This changes the focus from treating ailments to supporting ongoing health.
ROH: Where does the data come from, where is it collected and stored, and how do you ensure accuracy and privacy?
RJ: We should consider data collection and storage issues in two steps: now and in the future.
Currently, most of the data is collected and stored by health care providers and payers. This data is collected during patient visits to a clinic or hospital and at various imaging and laboratories. There used to be and still are incompatible record systems even among the same healthcare providers. That situation is improving but only incrementally because it is controlled mainly through business issues rather than health issues. Patients have no or tedious access to their own data. Privacy is managed by hospitals and payers and is used to limit control and access by patients and their agents.
Increasingly users are collecting their data via wearable devices and mobile phones. This data is collected outside traditional healthcare boundaries. Such data were not available to health care providers. More importantly, providers have been reluctant to integrate or look at this data. There are clear boundaries between Electronic Health Records (EHR) and regular data perpetually collected by users, commonly called User Generated Data (UGD). The acceptance of user-generated data or content within healthcare is increasing. Even regulatory organizations are open to such data. Some companies, notably Apple and Google, are creating data stores to collect an individual’s data from disparate sources and make it available at the user’s request.
The acceptance of user-generated data or content within healthcare is increasing.
Today, many people are developing Personal Health Records that will be under the control of the individual. These records will also be able to assimilate EHR data providing longitudinal data for the person from every possible source. Such data collection is essential to building a high-quality personal model for personalized and preventive approaches to medicine.
ROH: How can this data be used to predict the future health of individuals?
RJ: Everyone is unique because of genetics, environment, and lifestyle. Everyone also reacts differently to similar lifestyle factors and the timing of those. So, the essential task for predicting future health states is identifying and preventing potential problems at the individual level. A precise model of the individual’s body could guide potential lifestyle factors and provide foreseen health and medical needs.
To build a personal model to help prediction and prevention, one needs to collect data related to all inputs, outputs, and contexts for the system. Collecting 24/7 data related to lifestyle, environment, biomarkers, and other health-related information is vital. Collecting this data and using Machine Learning and Artificial Intelligence tools for event mining makes it possible to build a person’s model. Using their current health state, personal model, and potential inputs, it is possible to predict future health states. Thus, this model can guide a person in lifestyle inputs, environment control, and medicine to achieve desirable health.
ROH: Why should Medicine change its focus from a treatment and episodic disease or illness approach to Predictive, Preventative, Personalized, and Participatory (P4)?
RJ: Traditionally, healthcare and medicine have been episodic and reactive. During illness, data is collected to diagnose the disease and secondarily understand the cause. There is little or no proactive focus on maintaining and monitoring the ongoing health, lifestyle, and behaviors specific to that individual for comparison. Personalization promotes patient participation and should extend into environmental factors, triggers, reactions, and emotional or behavioral concerns impacting everyday life.
A Predictive, Preventative, Personalized, and Participatory approach, along with the aid of technology, provides an opportunity for a unique insight into what is “health” for an individual that far exceeds our current understanding.
A Predictive, Preventative, Personalized, and Participatory approach, along with the aid of technology, provides an opportunity for a unique insight into what is “health” for an individual that far exceeds our current understanding.
ROH: Describe an approach to patient compliance and adherence challenges, and what kind of data could be actionable info?
RJ: Patient compliance and adherence have two crucial components: reminders and behavior change. Reminders are essential to ensure people take the right actions at the right time. This may be related to medication, food, exercise, relaxation, or sleep.
Behavior change is challenging as people adopt habits and routines in life and are very averse to changes. Factors resulting in behavior change depend upon the individual. In building a personal model, data should also be collected on the person and related to behavior change. This will help create a personal behavior model for compliance and adherence and select the right approach for advising the person.
ROH: What devices, technology, data, etc., have the potential to modify real-time patient behavior and improve quality of life positively?
RJ: The most common devices for interacting with users are their phone and watch. These devices are readily available, provide the correct information at the right time, and collect compliance information perpetually. It is very similar to that used to provide personal health guidance. Continuous measurements and guidance are provided, and a user’s compliance behavior (and encouragement) is monitored and modeled.
ROH: How do you foresee diverse providers and services throughout healthcare having access to this data and collaborating to integrate it into practice to transform health for all effectively?
RJ: Healthcare providers have always been interested in the lifestyle-related information of their patients, particularly those facing chronic issues like diabetes. However, their food and exercise logs were not very accurate. Today, there is the opportunity to prepare objective, detailed diaries of lifestyle. And we are seeing increased interest in user-generated data to supplement office visits.
Today, there is the opportunity to prepare objective, detailed diaries of lifestyle. And we are seeing increased interest in user-generated data to supplement office visits.
Recently, the pandemic brought a significant change in the acceptance of remote patient interactions. Telemedicine and hospital at home were used throughout the country and are used now. Personal-related technology plays an important role. We also see a trend of new healthcare practitioners promoting acceptance of these emerging technologies.
ROH: You provide very optimistic predictions regarding data and healthcare! Where do you see the challenges ahead to make this reality, and how do you overcome them?
RJ: The major challenge is not the progress in technology and infrastructure but within business interests and legacy systems. Existing systems are incentivized to maintain the status quo and make only incremental improvements. This contributes to the high cost of US healthcare and the inefficiencies and ineffectiveness in the system.
The major challenge is not the progress in technology and infrastructure but within business interests and legacy systems.
The global situation is building rapidly towards adopting a new perspective on health. As mentioned within the WHO constitution, basic health should be provided regardless of the social status of every individual. The Internet provides access to knowledge, and mobile technology empowers communication globally. Health is the next frontier where data will bring even more transformative effects to human society.
About Ramesh Jain
Ramesh Jain is an entrepreneur, researcher, and educator. He is passionate about transforming health using technology. He is building a Personal Health Navigator (PHN) to give any individual the proper guidance at the right time and form. PHN is now imminent using cybernetic principles. It utilizes sensors, artificial intelligence, multimodal computing, and health sciences for guiding individuals as and when needed in their lifestyle actions and health-related needs. As a Fellow of AAAS, ACM, IEEE, AAAI, IAPR, and SPIE, he has co-founded several companies. After engaging in AI, multimedia, and social media research, he addressed health-related solutions to design a PHN. He is the founding Director of the Institute for Future Health at UCI (https://futurehealth.uci.edu/). He is currently associated with the University of California, Irvine; Ashoka University, Sonipat (India); Simula Labs, Oslo (Norway); Personicle.org, HealthUnity.org, Zepp Health, and DiaNavi.