RamaOnHealthcare July 28, 2023
Life After Practice & Lessons Learned
Bio Brief: Dr. Venkit S. Iyer is a board-certified surgeon, Fellow of the American College of Surgeons (FACS), Fellow of the Royal College of Physicians and Surgeons of Canada (FRCS-C), and Fellow of the International College of Surgeons (FICS). He has held leadership and teaching positions and provides lectures.
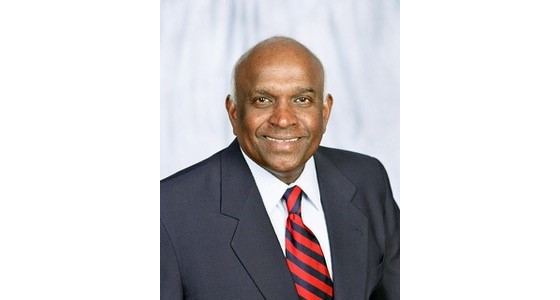
Dr. Venkit S. Iyer, MD, FACS, Surgeon and Author
RamaOnHealthcare (ROH): Dr. Iyer, you have quite an interesting story. Please tell us a bit about yourself.
Dr. Venkit S. Iyer (Dr. VI): Thank you for giving me an opportunity to be a participant in this forum. I was born in India, went to medical school there, and came to the US to obtain further training in surgery. Fortunately, I obtained a faculty position in the same hospital after training. A few years later, I started a private practice in general and vascular surgery. After thirty years of practice, I retired and have participated in various medical missions abroad and written books, and given lectures related to health care.
ROH: How has healthcare changed from the time you started working as a doctor fifty years ago, and where do you see it going?
Dr. VI: There has been remarkable progress in technology, science, and healthcare! Things have changed – significantly! Consider practicing today without CT scans, ultrasounds, MRI scans, angiograms, various endoscopic procedures, laparoscopic procedures, electronic medical records, and robotics! Numerous new vaccines and medications have been developed and changed the management of cancer care, heart disease, and stroke. Imagine getting through the day without cell phones, social media, personal computers, or the Internet and not having immediate access to legions of information! And it is not just bedside patient care – the means and methods of getting work accomplished have also radically changed.
I foresee science and technology continuing to make huge progress in the future. Much more automation and simplification can be expected. Fields of genetics and gene therapy, and molecular biology are going to explode. Many of the diseases that we consider incurable today can be eliminated. The longevity of the human race will be increased – and it will also bring in new sets of problems for us to handle.
Fields of genetics and gene therapy, and molecular biology are going to explode.
ROH: How do artificial intelligence and Chat GPT influence health care?
Dr. VI: Artificial intelligence and Chat GPT have been receiving ample press lately. And they are, rightfully, game changers. AI-incorporated changes will be felt throughout society. For example, the time spent reading medical images and generating reports will be reduced to a fraction of what it takes now.
We can look forward to earlier and more accurate recognition of malignancies, prediction of illnesses, virtual individual custom-made images of body organs and pathologies to facilitate practice surgery before the actual surgery, and reduced errors.
On the surgical side – Surgeons can expect warnings of potential injuries, better dissections, improved predictions of operating time, and better predictions of the outcome of surgery based on individual patients’ risk factors. In short, they can expect fewer surprises on the table. Likewise, Administrators will be able to streamline the workforce, improve the efficiency of daily operations, predict revenues, and improve profits. Primary care physicians will use smarter electronic medical records, reduce errors, increase time spent with patients, and show empathy to patients.
ROH: What challenges and problems do you see in healthcare in the US?
The US healthcare system has many positives and negatives. Technology is more advanced than most countries, but the money spent is also huge. However, the outcome and results are worse than in many other countries. No one seems to be happy with the situation. For the patients, it is too expensive, insurance companies dictate care, and delivery of care is not equitable or affordable. Many patients consider healthcare as impersonal, formal, and detached, and leaves them without a sense of direction.
Many patients consider healthcare as impersonal, formal, and detached, and leaves them without a sense of direction.
Physicians feel overworked, over-regulated, burned out, forced to be employees in some fashion, with limited, if any, independence, and facing mountains of regulations. Administrators are focused on the business of healthcare, and the overall focus appears to be short-term fixes and instant gratification rather than patient welfare and satisfaction. Furthermore, litigation and medical malpractice, cost of care, and over-specialization lead to defensive medicine with unnecessary tests and procedures. Healthcare has become more of a business than a profession. Solutions are few, and the options are precarious.
Healthcare has become more of a business than a profession.
ROH: Explain more about the fragmentation of health care.
Dr. VI: Years ago, the primary care physician oversaw the health care of the patient. The patient was referred to specialists only when needed. At that time, all the tests were coordinated through the Primary Care Physician, patients were followed daily when hospitalized, and there was trust and loyalty between the patient and doctor. Currently, much of this has changed, and the patients are often floating in a rudderless boat. Most Primary Care Physicians do not go to hospitals, and they work a fixed number of hours in their offices. After hours or in emergencies, patients go to walk-in- clinics or emergency rooms, and when admitted, they are seen by Hospitalists who work as employees within the hospitals. When an intervention or procedure is needed, often, they are provided by an acute care Surgeon, Interventional Radiologist, or Cardiologist, who again work mostly inside the hospitals. Once the immediate intervention is over, follow-up care is in unknown hands. Very often, it may be a Home Health Nurse arranged by the Hospitalist upon discharge. When the patient needs a question clarified or needs follow-up medical attention, they end up going back to the emergency room, and the cycle starts over. This time it could very well be another provider, who must look up the medical records for past information. No one knows who you are, you are just another number in the system. There is no single Physician in charge. The continuity of care is broken and desperately needs repair!
The continuity of care is broken and desperately needs repair!
ROH: What advice might you have for someone considering a medical or surgical career today?
Dr. VI: If you have the passion, then do it! We need you! Otherwise, analyze the positives and negatives before you choose. On the positive side, it is a noble profession where you can help fellow humans, save lives, and have a meaningful career, with a wide variety of choices in specialization. There are opportunities to work anywhere in the world and have a decent income and enjoy an upper-middle-class life. On the negative side, it takes years of education, training, and hard work to start actual practice. Most physicians are employees in some fashion, with a loss of independence, subject to many rules and regulations, and get burned out by midlife. The high risk of medical malpractice, defensive medicine, financial concerns, shifting paradigms in technology and protocols, and over-expectations by patients, are all issues that can lead to poor personal lifestyles.
ROH: Please tell us about your books, why did you decide to write, and how do you join the art and science within healthcare?:
Dr. VI: The first book is titled “Decision Making in Clinical Surgery”. It is a guidebook for junior surgeons and medical students discussing common surgical problems they encounter during rounds or in the clinic, written in a simple easy-to-read format, with a symptom-based or problem-based approach. The second book is “Aging Well and Reaching Beyond”. It is for general reading by all, explaining good health measures, wellness measures, preventive health care, elder care, and end-of-life issues. The more recent book, “The Clinic” is based on gene therapy and assisted reproductive technology and written as fiction for easy reading by all. The fourth book is “Geriatrics Handbook”, written as a sequel to the second book. This contains more medical information, a list of medications, and the care of elders. It is good for medical students, nurses, and paramedical personnel, as well as for general reading.
Currently, the first book is being revised and updated for its second edition. I am hoping to have it available by the end of the year. I have other projects in various stages of development as well.
More about Dr. Iyer: I am married and have three daughters and five grandchildren. When I am not reading or writing books and articles, I enjoy tennis, golf, and participating in local community activities. I also provide a variety of lectures regarding healthcare.
More information regarding my four books can be found on my website at https://venkitiyer.com





